Obstructive Sleep Apnea (OSA) is one of the most common and often underdiagnosed sleep disorders in the United States. It’s estimated that 30 million Americans live with OSA, many without even knowing it. OSA disrupts breathing during sleep which puts serious strain on the body which can lead to developing heart disease, high blood pressure, diabetes, depression, and other bodily complications.
Despite the well documented risks, many patients delay or avoid treatment. Perhaps its fear, uncertainty, misconceptions, or just the idea of wearing a mask at night that holds them back. But the truth is the real cost of waiting is far more significant than the perceived inconvenience of using a device at night.
Understanding OSA: What Happens During Sleep
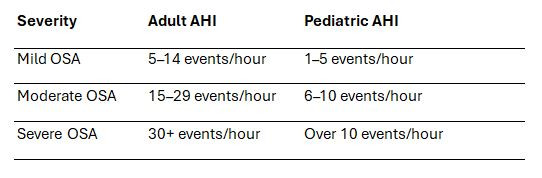
OSA is diagnosed through a sleep study. Sleep studies can be performed in a Sleep Lab or in the comfort of your own home. The study will measure several parameters such as Oxygen saturation, Heart Rate/Rhythm, Limb Movements, and how often you stop breathing during the night. The airway becomes obstructed while you sleep. Soft tissue in your throat and your tongue can occlude the airway. The amount of times this happens during the night, measured in 1 hour intervals is known as the Apnea-Hypopnea Index (AHI). The severity of your AHI is graded on the following scale.
If you’ve been diagnosed with OSA, or think you may have it, here’s why starting treatment sooner rather than later matters more than you may think.
What Happens When You Delay Treatment?
Sleep Apnea causes your airway to collapse repeatedly during sleep, cutting off airflow for seconds at a time. These “apneic events” happen over and over, sometimes hundreds of times a night. These interruptions reduce oxygen flow to the brain and body which triggers stress responses that increase the risk of:
- Hypertension (high blood pressure)
- Heart attack and stroke
- Type 2 diabetes
- Memory loss and cognitive decline
- Chronic fatigue and mood disorders
- Motor vehicle and workplace accidents

Why CPAP Therapy Works
The most common and effective treatment for mild, moderate, and severe OSA is Continuous Positive Airway Pressure (CPAP) therapy. A CPAP device gently delivers a steady stream of pressurized air through a mask while you sleep. This keeps the airway open during so you can breath normally throughout the night. No more gasping, snoring, or sudden wake ups.
Benefits of CPAP therapy include:
- Improved oxygenation and cardiovascular function
- Reduced risk of stroke and heart disease
- Better concentration, mood, and memory
- Improved energy levels and reduced daytime sleepiness
- Lower risk of accidents due to drowsy driving or microsleeps
Modern CPAP machines are smaller, quieter, and, more friendly, and more comfortable than ever before, with customizable masks and pressure settings to support user comfort and long-term compliance.
How Delaying Treatment Can Cost You (Literally)
The financial consequences of delaying CPAP therapy can be enormous both for individuals and society.
1. Higher Medical Bills
A long-term study published in Sleep found that patients who initiate CPAP therapy early have up to 50% lower healthcare costs over five years than those who delay or forgo treatment (Kapur et al., 2020). That’s because untreated sleep apnea contributes to more frequent ER visits, medication use, and hospitalizations.
2. Lost Productivity and Missed Work
Fatigue from poor sleep can reduce job performance, increase errors, and lead to absenteeism. In fact, untreated OSA leads to billions in lost workplace productivity every year.
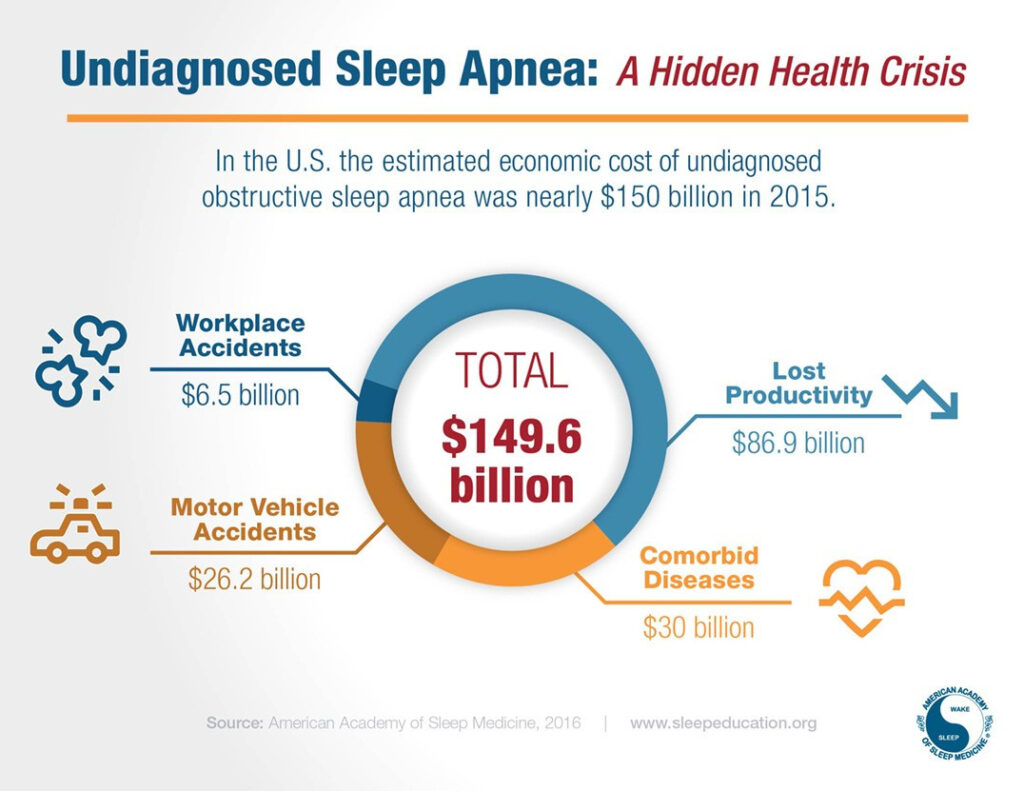
3. A $150 Billion National Burden
According to the American Academy of Sleep Medicine (AASM), undiagnosed sleep apnea costs the U.S. economy nearly $150 billion per year. This includes:
- $87 billion in lost productivity
- $26 billion from drowsy-driving crashes
- $6.5 billion from workplace accidents
- $30 billion in increased healthcare utilization
(Source: AASM, 2016 – Economic Burden of Undiagnosed Sleep Apnea)
These figures underscore that untreated sleep apnea isn’t just a personal health issue — it’s a public health and economic crisis.
The Insurance Catch: Use It or Lose It
Delaying CPAP therapy can also affect your insurance benefits. Many insurance companies require patients to demonstrate compliance by using the device a minimum of 4 hours a night on 70% of nights in a 30-day period. Failure to do so within a set period may lead to:
- Loss of coverage for the device (Device has to be returned)
- Denied claims for replacement supplies
- Out-of-pocket costs for rental or purchase
Worse, if your condition worsens while untreated, insurers may raise premiums or exclude coverage for related complications.
It’s Not Just About You
Sleep Apnea doesn’t just affect your health. It also impacts your relationships, your safety, and your overall quality of life. People often report:
- Chronic exhaustion that makes even daily tasks feel overwhelming
- Mood swings and irritability that strain personal relationships
- Snoring and restlessness that disrupt a partner’s sleep
- Drowsy driving, which increases the risk of car accidents
- Falling asleep during meetings or at church
OSA affects not just the person who has it, but everyone in their orbit ; spouses, children, coworkers, and communities.

It’s Never Too Late to Start
If you’ve been diagnosed with sleep apnea but haven’t started therapy, or if you gave up on CPAP after a rough start, know this: you’re not alone, and there are solutions.
Today’s CPAP systems offer options like:
- Auto-titrating (APAP) devices that adjust pressure automatically
- Heated humidification to reduce dryness and discomfort
- Slim, comfortable masks for a better fit and less claustrophobia
- Remote monitoring and support from DME providers and sleep coaches
If you have mild OSA, you may qualify for oral appliance therapy, or even a combination of both treatments.
Bottom line: Don’t Wait
The longer you delay CPAP therapy, the more you’re gambling with your health, finances, and daily well-being. But the good news is that sleep apnea is highly treatable, and starting therapy can drastically improve your life in just weeks.
Whether you’re newly diagnosed or have struggled with treatment in the past, now is the time to re-engage. Talk to your provider or DME partner about options that can help you succeed. Restful sleep isn’t just possible — it’s essential.
References:
- American Academy of Sleep Medicine. (2016). Economic burden of undiagnosed sleep apnea in U.S. is nearly $150B per year. Retrieved from https://aasm.org/economic-burden-of-undiagnosed-sleep-apnea-in-u-s-is-nearly-150b-per-year/
- American Medical Association. (2022). What doctors wish patients knew about sleep apnea. Retrieved from https://www.ama-assn.org/delivering-care/public-health/what-doctors-wish-patients-knew-about-sleep-apnea
- Kapur, V.K., et al. (2020). Health Care Utilization and Costs Among Patients With Obstructive Sleep Apnea Using CPAP Therapy. Sleep, 43(2). https://pubmed.ncbi.nlm.nih.gov/37964440/